Claims
Claims applies only to B2C users.
Use the Claims screens to view, submit, and track reimbursement requests for eligible medical expenses.
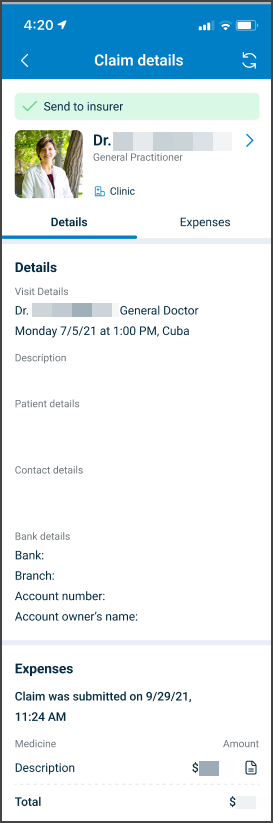
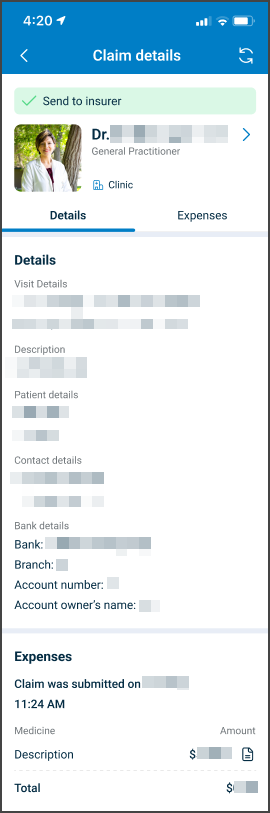
This screen includes
- Visit Details that show the related appointment.
- Patient details associated with the claim.
- Contact details for follow-up.
- Bank details used for reimbursement.
- An Expenses section that lists submitted expense items and totals.
- A submission timestamp and claim status.
Workflow
This sequence describes how a patient creates, manages, and tracks a claim.
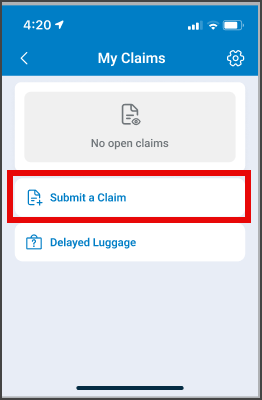
Create a Claim
- Open My Claims.
- Select Submit a Claim.
- In the Claim Form, enter the required information.
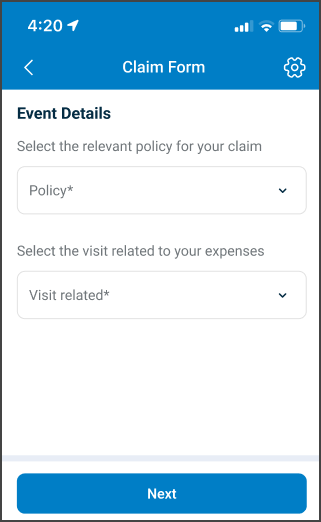
- Select Next to continue.
After submission, the claim becomes read-only.
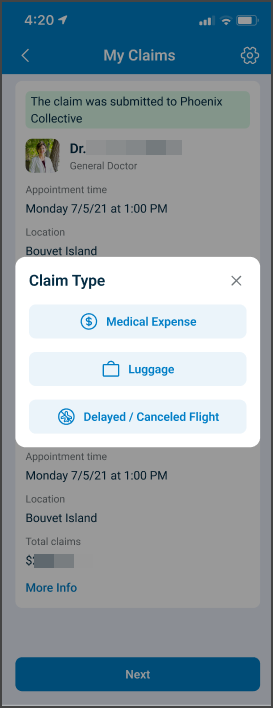
Manage a Claim
- Go to My Claims.
- Under Claim Type, select the relevant claim.
- Review the claim details, expenses, and total amount.
- To add an expense, select Add New Expense and enter the required information.
- Select Update to save the changes.
Track a Claim
If the claim receives approval, Air Doctor issues the reimbursement to the payment method on file for the appointment.
To request claim updates or status clarification, Air Doctor Customer Support.
Validations
| Scenario | App Behavior | SDK Output |
|---|---|---|
| Policy missing. | Blocks progression and highlights Policy. | Not applicable. |
| Related visit missing. | Blocks progression and highlights Visit related. | Not applicable. |
| Expense fields incomplete. | Disables Update and marks required fields. | Not applicable. |
| Claim submitted. | Locks all editable fields. | Not applicable. |
| Approved amount differs. | Shows the approved value in the summary. | Not applicable. |
| Expense deleted. | Updates the total requested amount. | Not applicable. |
Actions
| Scenario | App Behavior | SDK Output |
|---|---|---|
| Add New Expense. | Opens Expense Details. | Not applicable. |
| Update on expense. | Saves changes and returns to the claim form. | Not applicable. |
| Remove on expense. | Deletes the expense from the claim. | Not applicable. |
| Submit Claim. | Submits the claim and displays confirmation. | Not applicable. |
| Status becomes Clarification. | Enables updates and document uploads. | Not applicable. |
| Status becomes Internally Paid. | Sets the claim to read-only. | Not applicable. |
Endpoint Resources
Claims List
PUT
/claims
This endpoint returns the claims list screen configuration for the current patient.
Show Claim Details
PUT
/claims/details
This endpoint returns the claim details screen configuration for the selected appointment revision.
Update claim details
PATCH
/claims/details/update
This endpoint returns updates for the claim details screen for the specified appointment revision.
Show More Claims
PATCH
/claims/more
This endpoint returns incremental updates that extend the claims list for the current patient.
Update Claims List
PATCH
/claims/update
This endpoint returns incremental updates that refresh existing claim cards for the current patient.